Page 4 - Carotid and peripheral vascular interventions textbook
P. 4
CAROTID AND PERIPHERAL VASCULAR INTERVENTIONS: STEP-BY-STEP
Paravertebral
plexus
Vertebral v.
Lt anterior jugular v.
Rt anterior jugular v. Lt internal jugular v.
Rt internal jugular vein Ant. jugular arch
Lt external
Left external
jugular vein jugular v.
Rt superior intercostal
v.
Lt subclabian v.
Rt internal mammary v.
Lt superior
SVC
Lateral intercostal v.
thoracic v.
Lt thoracic v.
Posterior
intercostal v. Lt internal mammary v.
Azygous
v. Accessory
hemiazygous v.
Anterior
intercostal v.
Hemiazygous
v.
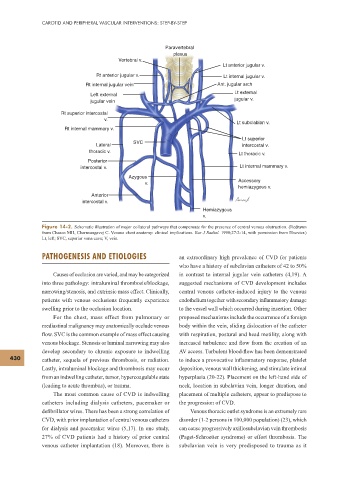
Figure 14-2. Schematic illustration of major collateral pathways that compensate for the presence of central venous obstruction. (Redrawn
from Chasen MH, Charnsangavej C. Venous chest anatomy: clinical implications. Eur J Radiol. 1998;27:2-14, with permission from Elsevier.)
Lt, left; SVC, superior vena cava; V, vein.
PATHOGENESIS AND ETIOLOGIES an extraordinary high prevalence of CVD for patients
who have a history of subclavian catheters of 42 to 50%
Causes of occlusion are varied, and may be categorized in contrast to internal jugular vein catheters (4,19). A
into three pathology: intraluminal thrombosis/blockage, suggested mechanisms of CVD development includes
narrowing/stenosis, and extrinsic mass effect. Clinically, central venous catheter-induced injury to the venous
patients with venous occlusions frequently experience endothelium together with secondary inf ammatory damage
swelling prior to the occlusion location. to the vessel wall which occurred during insertion. Other
For the chest, mass effect from pulmonary or proposed mechanisms include the occurrence of a foreign
mediastinal malignancy may anatomically occlude venous body within the vein, sliding dislocation of the catheter
f ow. SVC is the common example of mass effect causing with respiration, postural and head motility, along with
venous blockage. Stenosis or luminal narrowing may also increased turbulence and f ow from the creation of an
develop secondary to chronic exposure to indwelling AV access. Turbulent blood-f ow has been demonstrated
430 catheter, sequela of previous thrombosis, or radiation. to induce a provocative inf ammatory response, platelet
Lastly, intraluminal blockage and thrombosis may occur deposition, venous wall thickening, and stimulate intimal
from an indwelling catheter, tumor, hypercoagulable state hyperplasia (20-22). Placement on the left-hand side of
(leading to acute thrombus), or trauma. neck, location in subclavian vein, longer duration, and
The most common cause of CVD is indwelling placement of multiple catheters, appear to predispose to
catheters including dialysis catheters, pacemaker or the progression of CVD.
def brillator wires. There has been a strong correlation of Venous thoracic outlet syndrome is an extremely rare
CVD, with prior implantation of central venous catheters disorder (1-2 persons in 100,000 population) (23), which
for dialysis and pacemaker wires (5,17). In one study, can cause progressively axillosubclavian vein thrombosis
27% of CVD patients had a history of prior central (Paget-Schroetter syndrome) or effort thrombosis. The
venous catheter implantation (18). Moreover, there is subclavian vein is very predisposed to trauma as it